
Article | Jun 2020
Responding to the COVID-19 Crisis: Healthcare Board and Human Resource Perspectives
Learnings from both CHROs and healthcare trustees on the compensation challenges they are facing during the pandemic.
On April 21st Pearl Meyer hosted a virtual peer exchange among five healthcare provider CHROs, and on May 19th we hosted another virtual peer exchange, this time among seven healthcare provider board directors. In total, the 12 individuals represented seven acute care organizations: two urban academic medical systems ($1.5B and $3B in revenue), an urban public safety net healthcare system ($1.2B revenue), two urban integrated delivery systems ($2.2B and $2.7B in revenue), and two semi-rural regional medical centers (both about $350M in revenue). The seven organizations are located in six states: Florida, Illinois, Massachusetts, Ohio, Texas, and Virginia.
Discussion Topics
All were all invited to share questions and discuss challenges forced by the ongoing C-19 pandemic in the United States. Prior to the two sessions, Pearl Meyer prepared and shared a list of discussion topics and participants approved of the lists in advance.
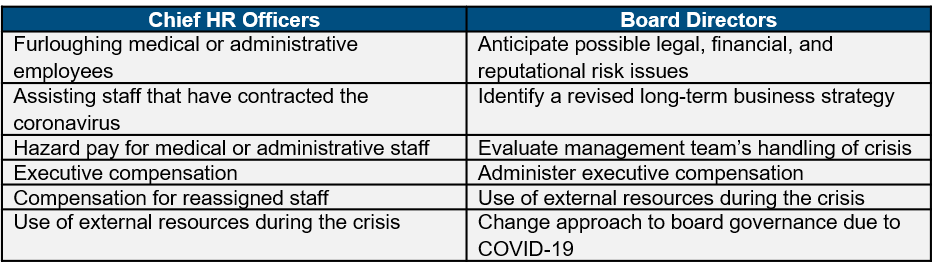
While the perspective of board directors is commonly thought to be more strategic and that of HR executives more operational, the two groups were focused on similar issues. To their credit, the contributions from the HR leaders and board directors affiliated with the same organizations were very similar!
Shared Experiences
CHROs and directors alike all said that their organization is experiencing reduction in revenue due to the discontinuation elective procedures and most ambulatory services. All are either engaged in identifying or executing workforce and expense reduction activities. Geographic location seems to make a difference with regard to the progress they are making in cost reduction as some were impacted by a surge in COVID-19 cases sooner than others. Those located in geographies that experienced the pandemic early on are taking more aggressive action around cost reduction than those located in areas only experiencing the beginning of the infection curve. HR executives from organizations in earlier stages of reacting to the pandemic were able to ask direct questions of their senior HR peers at institutions first impacted by the pandemic. The reduction of IT-related costs is a concern shared by all the organizations which participated in the sessions. One director said that “everything is being looked at unless it relates to patient-facing activities.”
None of the organizations represented in either peer exchange are providing hazard pay. All agreed that healthcare employees recognize that working in hazardous conditions is to be expected and part of the job. However, one HR executive mentioned their organization provides up to two weeks of pay for employees quarantined due to COVID-19 exposure at the hospital. Several CHROs shared that they’ve had employees file worker’s compensation claims due to COVID-19 exposure at their workplace. An HR executive from one of the larger urban organizations said they provide paid housing for employees treating COVID-19 patients who have compromised family members at home, and another mentioned paid childcare expenses for their employees. One of the directors observed that furloughs and layoffs often result in increased duties for remaining staff, and in response one of the other directors shared that their organization has started to provide extra childcare and free/reduced cost food for employees. That same organization has also set up a crisis fund for staff in need.
Employment Costs
The healthcare system directors expressed concern over long-term sustainability and general cost savings, sharing that “even after the pandemic we will not return to easy street.” There was a lengthy conversation about the need to motivate the staff to cut costs. Interestingly, three of the health system CHROs shared that their organizations have created cost centers to track all expenses directly related to COVID-19.
Several of the HR executives described a number of creative workforce management approaches, including:
- Employees working reduced hours for reduced pay but maintaining their benefits
- Telework for employees whose jobs enable them to do so
- Reducing pay rather than terminating or furloughing employees
- Job-sharing where two part-time employees can share one full-time role; both are paid a part-time wage and continue to receive benefits
- Job shifting (e.g., a business manager working in patient transport), but the employee receives pay as if in their original role
- Creation of staff pools where employees whose own jobs are nonessential can help out temporarily in other areas; one organization has a full-time staffing coordinator to manage this process
One CHRO mentioned that each department has a goal to reduce administrative expenses by 20% without resorting to furloughs or layoffs. That particular organization’s employees are encouraged to use existing PTO because reducing their PTO bank reduces the liability on the system’s balance sheet. Another HR executive mentioned that their organization will achieve a 20% reduction in payroll costs by having employees work and get paid for four days a week versus five days. One CHRO’s organization offers voluntary furloughs in two-week increments based on seniority, which the participant said has been a popular option for their employees.
During the board session all directors talked about their organizations’ need to reduce people costs. One instituted a voluntary retirement program and a voluntary unpaid sabbatical program.
Base Salaries
The board directors and the HR executives all engaged in lengthy discussions concerning direct compensation costs, and how executive and employee compensation is being managed during the COVID-19 crisis. Among both groups, base salaries were described as an important cost-savings strategy. Accordingly, all of the HR participants said that their organizations have suspended merit-based salary increases for 2020.
Several of the HR executives discussed implementing executive pay cuts as well as director pay cuts (for organizations with paid directorships). The CHROs uniformly shared that the majority of these executive pay adjustments are voluntary, with CEOs commonly taking the largest base salary reductions, generally ranging from 20% to 50% of base salary. Reductions for other c-suite executive and senior management positions were described as being between 15% and 30%. The organizations seemed to be evenly divided on longevity; those for whom the cuts are finite will either resume full pay or reevaluate after 90 days while the others’ reductions are “indefinite.” The board directors described base salary cuts among executives as very similar to those discussed by the CHROs, even those from different organizations.
Pearl Meyer observed that those organizations whose executives forfeited a portion of their base salary are the same organizations that furloughed employees without pay. Is it possible that these executives (and their boards) decided that they should “lead by example” or in some way appear to share in the sacrifice?
Variable Pay
All peer exchange participants were asked how their organizations plan to address variable compensation programs in light of diminished financial performance and therefore reduced or nonexistent incentive awards. Both sessions included very interesting conversations about variable pay decisions during the healthcare crisis. Several of the directors volunteered that their boards decided to suspend all bonus plans for 2020, saying that “all people will take a hit.” All agreed that the current situation “is not a good time for variable compensation awards to be paid out.”
None of the CHROs expected their executive and non-executive incentive plans to pay out. Most said that they are operating on a “wait and see” basis and feel that it’s just too early to make consequential decisions about annual or long-term incentive arrangements. Every HR executive said that their organizations would be “out of the money” on most financial measures, including those that are part of their executive incentive plans.
Several directors volunteered that their boards are challenged about whether to establish temporary executive and management incentive opportunities around cost reduction. One director said that “incentive plans can motivate expense reduction activities” but asked “should we pay bonuses during a time of very poor margins and so many layoffs?” Several of the directors asked the group whether the executive team’s overall response to the pandemic provides sufficient justification for awarding incentive payments for 2020.
The peer exchange participants whose organizations have long-term incentives (LTI) said that they are waiting to see how the year turns out but that they likely will not pay out on any open LTI grant cycles for 2020.
Benefits
HR and board participants all said that they are very concerned about employees being able to retain their health insurance benefits. Most said that if their furloughed employees receive medical care their insurance can be billed direct or the employees can go into arrears with their premiums and settle their accounts when they return to work. Several CHROs shared that they have suspended the company 401(k) matching contribution. All of the HR participants said that they are looking at the retirement plan provisions in the CARES Act to determine whether/how to make changes to their plans to provide greater financial flexibility to their employees (e.g., loans, early distributions, etc.). Several have applied or are in the process of applying for funding through the CARES Act, but CARES Act funds are not available to public safety net hospitals.
Summary
Clearly workforce staffing and cost containment solutions are not one-size-fits-all. Because Pearl Meyer is familiar with the actual organizations represented in both peer exchange sessions, we observed that most of the approaches described by the directors and CHROs appear to align with their individual organizations’ business model, culture, financial health, and location. Those institutions more financially reliant on suspended voluntary procedures and ambulatory services are more profoundly impacted by the pandemic and are making bigger cost cuts, including furloughing. Those located in states whose economies are “opening up” before others will be resuming some of the suspended services immediately, which presumably will put them back on firmer financial footing and allow them to roll back some cost-cutting initiatives.